S1: Welcome in San Diego , it's Jade Hindman. Today we share the stories of people living with long Covid and the need for research. This is KPBS Midday Edition. Connecting our communities through conversation. Welcome back to KPBS Midday Edition. I'm Jade Hindman. More than five years after the Covid 19 pandemic began , many San Diegans are still living with the long term effects. KPBS health reporter Heidi DeMarco says long covids lasting health impacts are often invisible and misunderstood.
S2: Jason Reitman is lucky to be alive after contracting Covid in December 2020. He spent 70 days in a coma.
S3: I text my wife , I said , I've got to go to sleep for a while. I love you , I'll. I'll talk to you when I wake up.
S2: Reisman is a special agent with Homeland Security. He caught Covid at work before the vaccine was available.
S3: As a result , I have some residuals that I'm still seeking treatment for.
S2: There's no clear number on how many people in San Diego are living with long Covid. Experts say it's hard to track. Many patients aren't diagnosed or don't realize what's wrong.
S4: There's people who have cognizant of issues where they're they're forgetting things. They have what they call brain fog. There's people who have endurance issues. There's people who have mainly respiratory issues. There's people who have cardiac issues.
S2: Christopher Malloy manages the la mesa Rehab in East County. He says they've treated more than 120 long Covid patients since the pandemic began. They combine pulmonary therapy and physical rehab.
S4: People come in in tears Care , saying , I just want to go back to work , but I'm not the same anymore. I don't have the endurance. I don't have the strength.
S2: Doctor Tammy Peavy is the rehabs clinical director. She says there is no official test to diagnose the condition or a standardized treatment plan for long Covid , which can impact nearly every system in the body. She says too often , patients are referred to physical therapy without being properly evaluated for breathing issues.
S5: So I think it's really important to send the message out to doctors that if a patient comes in with shortness of breath , do not be afraid to send them to pulmonary rehab.
S2: La mesa rehab is one of only five clinics in San Diego County.
S5: I think the saddest thing is there's only 300 clinics like this in the entire United States. We should be more prepared than that. And we should certainly be taking better care of the patients who haven't recovered from the Covid.
S2: Deborah Franklin still deals with blurry vision , body pain , loss of taste and smell , and a relentless cough.
S6: I have had long Covid since December 2021. I had like three different kinds of inhalers.
S2: Rehab helped her realize she wasn't alone.
S6: As I got to see other people with it , because the doctors kept saying , well , no one else has this.
S2: Another challenge. Health coverage.
S4: People being denied worker's comp.
S2: California Senate Bill 1159 used to make it easier for people to get worker's comp if they caught Covid on the job. But that protection expired in 2024. Now workers have to prove they got Covid at work. PV says that makes it tougher for long Covid patients to get coverage.
S5: They're only giving certain number of visits. We have to go back and ask for more visits. These are long term patients.
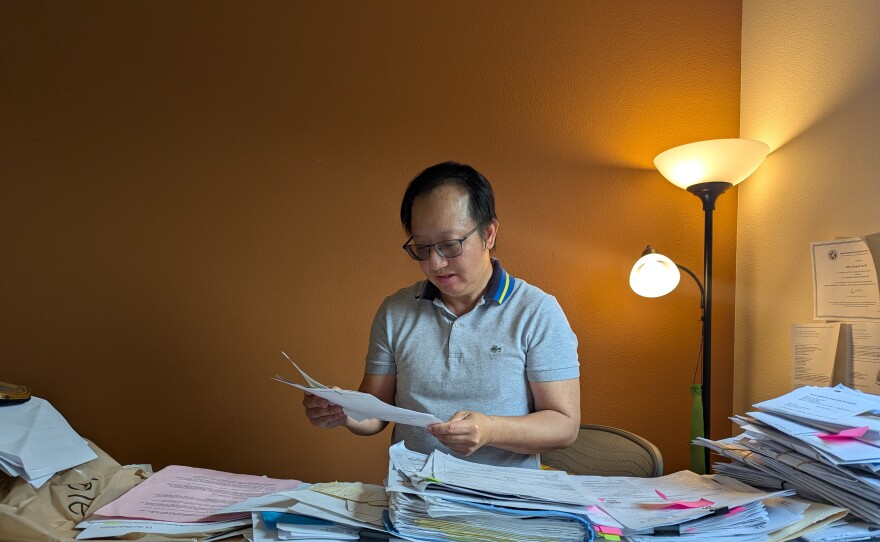
S2: Doctor Alan Lee is a psychiatrist.
S7: There's another medication that my doctor wants to prescribe me. It's 3000 a month.
S2: He says even with his medical background , it's hard to get care after being infected with Covid in 2022.
S7: One of the struggles is , of course , just working with insurance to try to get things authorized , because these treatments can be expensive , and especially for a novel illness where a lot of the treatments are not yet approved.
S2: After a heart rate monitor claim was denied by his insurance for not being filed properly. Allen says the company sent him to collections.
S7: As you can imagine , being really tired and everything like that. It's really hard to take care of these kind of things.
S2: Federal support for long Covid research is also dwindling. The Trump administration is planning to close the office for long Covid research and practice five years since the pandemic hit. Research , recovery and treatment for long Covid patients remains uncertain.
S6: But it's just been a long journey.
S2: Franklin might retire early.
S6: I'll have to wear a pamper to work because my cough is so aggressive. I really have to figure out if it's worth it.
S2: Reisman continues to fight for proper care.
S3: I was too stubborn to die , and I'm too stubborn not to get treated properly.
S2: Doctor Lee can't work anymore and now finds himself struggling to keep up with his kids. A few minutes on the playground can knock him out for up to 14 hours in bed.
S7: Regardless of how tired. I mean , these moments , they are , you know , you only have so long with with your children.
S2: With no clear roadmap. Health experts say long Covid patients are left to navigate a system that is still learning how to manage this complex condition.
S1: That was KPBS health reporter Heidi DeMarco. Heidi , thanks for joining us today.
S2: Thanks , Jade. It's great to be here.
S1: Glad to have you. So. Your story highlights the challenges , really , of living with long Covid and telling this story through the lens of people struggling with that.
S2: You know , one woman told me it's it's been a long , lonely journey , and they're suffering in silence. This is something that is not visible , like a broken leg where you , you know , can get comfort or support. It's there dealing with it behind closed doors. So it's it's an it's invisible. Wow.
S1: Wow. And it's been five years since Covid 19 became a pandemic. And yet the medical community is still trying to understand long Covid and all of the lingering effects that come along with it.
S2: It affects nearly every system of the body , and no two cases seem to be the same. So what works for one person might not work for another. So that makes it incredibly difficult to study , to diagnose , and to treat patients.
S1: Well , as you mentioned , I mean , it is really striking how differently this can affect people. Can you talk more about those wide ranging symptoms ? Sure.
S2: A lot of people , you know , have different symptoms. Some have brain fog. Others deal with lung and breathing issues. Some have cardiac issues and they can't tolerate physical activity. I spoke with one doctor who a few minutes , you know , on the playground with his kids , sends them to bed for about 14 hours. So all all these symptoms just they range. And so the treatments also range. They're not it's not the same for everybody.
S1: Well , so in your report we heard from two clinicians treating patients with long Covid. Tell me about those treatments.
S2: So right now most people are being treated based on their symptoms. At this particular clinic that I went to the combined pulmonary rehab with physical therapy. But a lot of , you know , different clinics are using , you know , physical rehab for fatigue and weakness , um , brain training to help with memory loss or brain fog and even olfactory retraining to help with loss of smell. But there's no standard yet , so it's very trial and error. This isn't an established disease like diabetes , where we know what treatment is needed once diagnosed.
S1: So there is this challenge to find the right treatments for people suffering from long Covid.
S2: Even when people finally get a diagnosis , they often can't get coverage for the care they need. Insurance companies , you know , question claims or deny equipment or don't approve enough visits. And that's especially hard for people who are already physically and mentally drained. And also in terms of specialty. Like here in San Diego , there are only five clinics that are treating long Covid patients well.
S1: And adding to the overall uncertainty surrounding long Covid comes new uncertainty on the future of research with all of the federal cuts. How might the cutbacks affect medical research and the treatment of people suffering from long Covid.
S2: Well , the closure of the Federal Office for long Covid research is a big blow. That office was coordinating national efforts , and losing it risks slowing progress , stalling clinical trials and , you know , delaying answers that these patients desperately need. And they feel that , you know , they're already struggling to get diagnosed and treated. And so if research dries up , the uncertainty around care and recovery just gets worse. So some of the folks that I spoke with , they just feel forgotten by the system. And these cuts , you know , reinforce that feeling.
S1: Well , you really tell the personal stories of people who are impacted by long Covid.
S2: They're trying to work , care for families or just get out of bed. And many aren't being properly diagnosed. So these stories help put a human face on what can feel like a distance , you know , a distance issue and helps these people feel less invisible.
S1:
S2: They didn't know what was wrong with her. She when they mentioned long Covid , it was a relief. But also she had no idea what it was about. But you know , she said she she appreciates when doctors just don't have the answer. And that's what's happening. They're going in. They're being diagnosed for , let's say , physical therapy. And it needs to be more comprehensive than that. Um , and so they just feel unheard. And the treatment they're getting sometimes isn't the right one.
S1:
S2: They said they want long Covid to be taken seriously , you know , by employers , insurers and the health system. They hope for research that leads to real answers and a system that doesn't make them fight so hard for care.
S1: I've been speaking with KPBS health reporter Heidi DeMarco. Heidi , thank you so much for your reporting.
S2: Thank you. Jade.
S1: Thanks for joining us today. If you missed anything , you can download KPBS Midday Edition on all podcast apps. Don't forget to watch Evening Edition tonight at five for in-depth reporting on San Diego issues. I'm your host , Jade Hindman. We'll chat again tomorrow. Have a great day , everyone.