MAUREEN CAVANAUGH: This is KPBS Midday Edition, I am Maureen Cavanaugh. Being injured in a car crash, a fall, or being the victim of a violent crime can leave you in need of a particular kind of hospital care. Healthcare professionals call these traumatic injuries, and various forms of trauma are the leading cause of death for Americans under the age of forty-five. Several decades ago, several members of the San Diego medical community decided to do something to reduce the number of trauma deaths, and this year they are celebrating the thirtieth anniversary of the San Diego trauma system. It has cut the number of trauma deaths in half, and it is one of the leading trauma care systems in the nation. I would like to welcome my guests. Doctor Michael Sise is Medical Director of the trauma unit at Scripps Mercy Hospital. Doctor Bruce Haynes is Medical Director at San Diego County Emergency Medical Services. Welcome to the program. Doctor Haynes, I read before the trauma system was put in place that people were badly injured in San Diego were just taken to the nearest hospital, what was wrong with that? DR. BRUCE HAYNES: What was wrong, even though you could have a good hospital, if there is no organization and rapid approach to the patient, a comprehensive approach to the initial diagnosis and treatment, people did not do as well as they should have. Some studies were done around the country, looking at preventable deaths, and they found that frequently there was a high number of deaths that could have been prevented. A study in San Diego showed a preventable death rate of 21%, 21% of people who died, it could potentially have been prevented. MAUREEN CAVANAUGH: I was wondering, if you could tell us the difference between a trauma hospital versus a traditional emergency room. DR. MICHAEL SISE: In San Diego, all of our hospitals are excellent. The difference between a trauma center and a hospital is not the resources, not the people, not the equipment many of our trauma centers have all of that. It is the organization of those personnel, equipment, resources, OR, cat scanners, to be able to promptly work up and treat the injured. All we do at a trauma center is put all of those resources together to measure and improve performance, and you get you care for by the right people at the right time as quickly as possible. MAUREEN CAVANAUGH: Doctor Haynes, how did the San Diego trauma system get started? DR. BRUCE HAYNES: There was discussion as there was elsewhere in California at the time, about this problem and whether or not it truly existed. A study was done that pointed in the direction that there was a problem, and a larger study was done that there were preventable or potentially preventable death rate of 21%. From there it was decided to institute the trauma system. MAUREEN CAVANAUGH: How many hospitals are part of the trauma system in San Diego? DR. BRUCE HAYNES: There are six, Scripps Mercy Hospital, Sharpe Memorial Hospital, Scripps La Jolla, Rady Children's Hospital, Palomar, and UCSD in Hillcrest. MAUREEN CAVANAUGH: What kinds of trauma cases do see most of? DR. MICHAEL SISE: We see all different causes of injury, but more and more as our population ages and we are living longer with heart disease and curable cancers, we're seeing more and more old folks who fall. The reality is, 25% of the citizens in San Diego County age sixty-five and older will fall this year. Once you get to ninety, I know a lot of folks who are ninety living relatively well, but it is almost a 100% fall rate. Those falls are associated with fractures, head injuries, and folks were not that healthy to start with, so it is becoming an increasingly challenging area for us, and an area for focus and improvement. MAUREEN CAVANAUGH: I have heard that in the thirty years that the system has been in place that the number of car crash victims has decreased. I guess that is the positive side of the number of trauma patients. DR. BRUCE HAYNES: It is, and it is partially due both to safer roads, and safer drivers, I would like to think that but I'm not convinced. And cars that are absolutely reengineered for safety and survival. We're seeing people walk away from cars that are destroyed, with relatively minor injuries. We used to kid in the old days, if you got in a car crash in the 60s or 70s, it would say ìtelorvehCî across your chest because that was Chevrolet spelled backwards, because the steering column would slam you right in the chest. Now, all engineered cars have zones of safety that protect you, airbags have been transformational in leading to survival. But it is still based on good, safe driving, with the assistance of new engineering. MAUREEN CAVANAUGH: What factors determine where in the system of trauma units that a patient will be taken? Is it the type of injury that they have suffered, or is it geographical? DR. MICHAEL SISE: It is geographical. Each of the five adult trauma centers has what we call a catch area, where if the patient is injured in that area they are taken to that center. The exception is the Rady Children's Hospital, where they get all of the injured children ages fourteen and younger in the County. MAUREEN CAVANAUGH: Would like you both to comment on my next question. A trauma system that has been as successful as the one that we have here in San Diego, it does not just happen. How much have the hospitals and medical professionals worked at refining this approach? DR. BRUCE HAYNES: Well, they've worked hard and they keep working. That is the thing that needs to be recognized about these people, the death rate from trauma, from potentially preventable deaths dropped down to under 3% and then down to under 1%. Over the last twenty years, the most severely injured patients, the death rate has gone down by 50%. It is a remarkable achievement. MAUREEN CAVANAUGH: How do the professionals work together? How does that actually work, among yourself and other doctors and healthcare professionals in the trauma system around San Diego? DR. MICHAEL SISE: Well, it works by measuring performance, literally. A lot of folks have said we probably should conduct medical practice like we're flying airplanes. I think it is instead like being a professional athlete, there are clearly hits, runs, and errors. The best athletes are those who can identify things not going well, make changes and still win the game. We measure everything, I've been taking trauma calls for twenty-seven years, and I can go back and show you a durable record of the moment I showed up compared to when every patient I responded to arrived, and when I showed up. That kind of measurement is unprecedented in care. We then generate the ability to identify opportunities for improvement. Unique to San Diego, right from day one in 1984 when we put the system together, all of the trauma centers agreed to meet with our tardy partners, and we have a great working relationship with the County partners. And we frankly discussed in peer-review, so it is protected, all of our errors and opportunities for improvement. Once a month we still need, review each other's care, designate what we want to talk about as an opportunity for improvement, and we learn from each other again and again and again. This is a contact sport, taking care of injured patients. You cannot be at this for any length of time without being humble, and without understanding that you have to continually train, and practice, and acquire new knowledge. San Diego is very fortunate that we have been able to do that going on thirty years and will continue to do it. MAUREEN CAVANAUGH: Can you give us an example of the kind of intervention that is being used now to keep patients alive, that is been developed by this trial and error collaboration? DR. MICHAEL SISE: It is interesting, we learned immediately from what was happening in the wars in Iraq and Afghanistan and brought those lessons home. We learned in Iraq and Afghanistan if someone was badly injured and bleeding, if they were talking to you and had a pulse, and were not actively bleeding, don't do anything until you get that person into the operating room and can clamp that artery or control hemorrhage because giving fluid or blood raises blood pressure and restarts hemorrhage. We brought that home, here in San Diego, right around 2007 throughout the system. It absolutely transformed the survival rate around major hemorrhage. In the past, we would give a lot of saline, saltwater, and blood cells. Now we give saline, plasma, and blood cell transfusions, they hold the saline, and in doing so we have cut down the instance of shock lung. People getting lungs full of fluid after being in shock. We don't see that anymore almost at all. People are surviving, in fact there was a great case that two of my colleagues took care of, a horrible car crash. The person had a crushed liver, most died, and was rushed to the operating room, we opened the abdomen and packed the liver, did the best we could to contain the bleeding, did the blood transfusion, took him back to the ICU, and really not expecting him to survive. My colleague, who had been into back of my other partner called a couple hours later and asked when did he die, and my colleague said he is doing just great. Those kinds of specific examples represent what we did in San Diego by working together, and looking for new ways to do things by importing proven and promising ways to treating patients to the home front. And now, San Diego benefits just like all of our warriors did. MAUREEN CAVANAUGH: Another aspect of the trauma system here in San Diego is that the different trauma centers have agreed not to compete against each other. How has that helped the overall trauma system? DR. BRUCE HAYNES: I think there is a field system of cooperation. Mike was talking about the case review reviewing the computer-generated things to look at, all of that, everybody is focused on the patient and doing better. They are not focused on competition between hospitals. MAUREEN CAVANAUGH: Because in other cities, people may be familiar with different trauma centers advertising, we have the best, center, we do not see that. You see different ads for hospitals, but you do not see that specific kind of competition, is that with the hospitals agreed not to do? DR. BRUCE HAYNES: Yes, that is part of our advertising policy and protocol. They have agreed to do that. I think that has worked out really well in keeping the spirit of cooperation up. MAUREEN CAVANAUGH: Are there still gaps in the trauma service in San Diego? DR. MICHAEL SISE: There are not gaps in the care of injured, but you cannot be at this business for any length of time without realizing how important prevention is. We're all at risk for cancer, heart disease, particularly if we have family history or just live long enough. But none of us, none of the members of our community need to be injured, it is entirely preventable. We're getting out in the immunity, working with law enforcement, schools, and other partners, looking at prevention. We would love to be out of business, no doubt about it. When you have a young child at home, you can walk into a room and figure out where that child could get into trouble. As trauma surgeons, we travel through our lives seeing risk everywhere. We can see what someone will get into. Equally importantly, their behaviors begin work on with our children, with each other, and with our seniors. Drug and alcohol use, dangerous driving, texting and driving, all of the things that we know can increase risk of injury. Our service to the community is not just to be there when you are injured, and try to get you back to your family, but to help you get the information make good decisions to avoid injury. MAUREEN CAVANAUGH: How is the system maintained in the county? Do all of the trauma centers collaborate by paying for it? Who pays for it? DR. BRUCE HAYNES: There are fees that come in as part of a state program in the County that support some of the infrastructure. That is one way. In general, the sport is really from fees from patients and the usual hospital charges, that sort of thing. MAUREEN CAVANAUGH: A quick last question, what will the future look like for the system? What can you see developing in the near future? DR. MICHAEL SISE: I think will continue what we have always done, learn, adapt, adjust, and deliver on that promise day and night to be there for the community. There are great youngsters coming along, some female surgeons, one of my new partners is a young mom in her 40s, a mom with two kids who is a rock star. She is the face of the fact that 50% of our surgeons and medical students are women. We are changing, and growing, and we will always be there for San Diego. MAUREEN CAVANAUGH: I want to thank you both for giving us such an in-depth look into this. I really appreciate it. Thank you both.
Being injured in a car crash, a fall, or being the victim of violent crime — can leave you in need of a particular kind of hospital care.
Health care professionals call those traumatic injuries and various forms of trauma are the leading cause of death among Americans under the age of 45.
Several decades ago, members of the San Diego medical community decided to do something to reduce the number of trauma deaths. This year, they're celebrating the 30th anniversary of the San Diego trauma system.
The system is considered one of the leading trauma systems in the nation and is credited with reducing the number of trauma deaths in half.
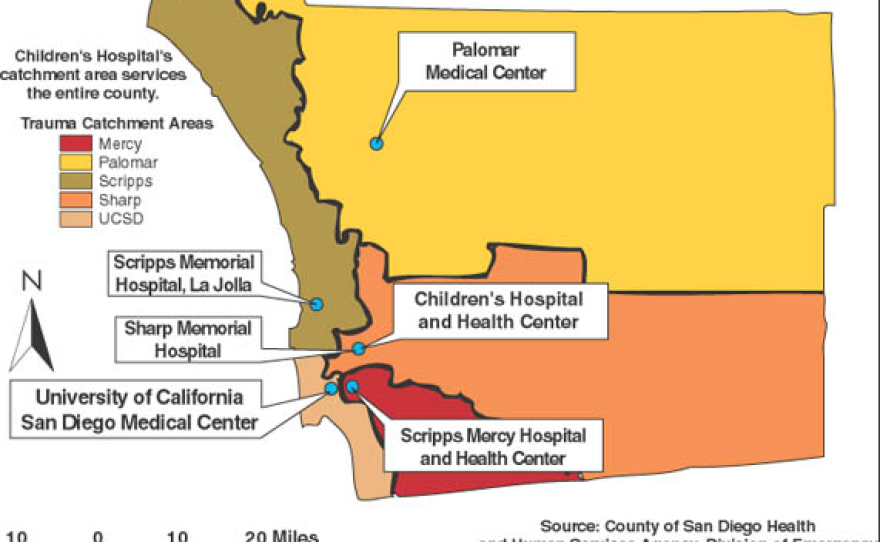
Six area hospitals make up the system.
• Rady Children’s Hospital
• Palomar Medical Center
• Scripps Memorial Hospital, La Jolla
• Scripps Mercy Hospital and Health Center
• Sharp Memorial Hospital
• UC San Diego Medical Center
Under the old system, trauma victims were taken to the nearest emergency room. But often times, county officials say, local hospitals lacked on-site trauma surgeons, specialists and resources to treat major traumatic injuries. Now, trauma victims in San Diego bypass community hospitals in favor of designated trauma centers.
In the past 30 years, about 250,000 injured patients have received vital trauma care in the region.