Second Of 2 Parts

Brain surgery is a team sport.
And for this operation at UC San Diego Medical Center in Hillcrest, Dr. Clark Chen has 10 people on his side.
But one of the most crucial players isn’t a doctor, nurse or technician — it’s the MRI machine.
Chen will rely on this machine and some special software to guide him every step of the way through this delicate procedure.
In the weeks leading up to the surgery, Chen used state-of-the-art imaging tools to help devise his plan of attack on the brain tumor.
Now it’s show time.
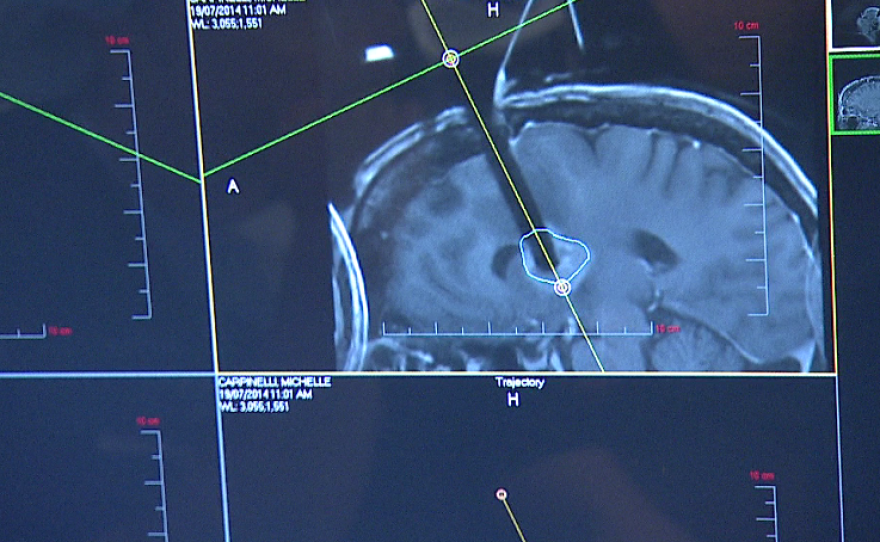
The patient, 52-year-old Michelle Carpinelli, has been put under anesthesia and a small hole has been drilled in her skull. Special instruments are mounted on her head to make sure Chen stays on the right path.
“This is exactly where we made the incision," Chen said, pointing to the computer monitor. "And in fact what we can also see, is to see this in three dimensions, looking at the MRIs superimposed onto the tumor.”
With conventional surgery, the neurosurgeon calculates where he’s supposed to be in the brain, and the equipment guides him there, but he doesn’t know precisely where he is.
In contrast, the 3-D brain scans help Chen get to the right spot with sub-millimeter accuracy.
“With real-time MRI, you could actually see the needle physically in the tumor, which is not something that is doable with conventional surgery," Chen pointed out.
Chen inserts the biopsy needle into Carpinelli’s brain.
Scans show he’s right on target. Chen extracts a couple of samples from the tumor.

“Send that to path, please. Take one more for permanent.”
“We’re getting two specimens, and we sent them now for pathology analysis," Chen explained. "And now we’re getting the scan to make sure at the site of the biopsy, that no harm is done.”
A few minutes later, the pathologist calls. He tells Chen the first sample was inconclusive for cancer.
“But you may want to consider getting us a second piece for permanent," the pathologist said.
“Well, we’re smack in the center of it, based on the MRI," Chen replied. "So take a look at the second one and see.”
“OK," the pathologist replies. "We’ll let you know.”
The second sample also comes back as inconclusive. So Chen goes back in the operating room and extracts other pieces of the tumor for the pathologist.
These samples eventually confirm what Chen suspected all along: The tumor is malignant.
Now it’s time to destroy it.
But first, Chen tests a flexible laser probe to make sure it’s working properly.
Then he slowly inserts it into Carpinelli’s brain.
“I feel now a very firm area," Chen said. "I know that’s the tumor. And I’m now inserting the probe into the tumor.”
This is a critical moment. Chen and his team do another brain scan to confirm that the laser is in exactly the right spot.
It’s all systems go.
From the control room, Chen fires up the laser with a foot pedal.
Using what’s called MRI thermography, Chen monitors the temperature within the tumor.
Chen carefully controls the laser, to make sure it’s not heating up other parts of the brain adjacent to the tumor.
After about five minutes, Chen gives the word.
“OK," he said, smiling. "I think we’re good."
A final scan tells the tale.
“So at the end of the surgery, we were able to visualize whether there’s any harm related to the surgery, which there isn’t," Chen explained, outside of the operating room. "And we’re also able to visualize that we’ve destroyed the entire tumor.”

The team wheels Carpinelli out of the operating room, and begins to wake her up.
“Can you wiggle your toes, dear? Good," a nurse said.
“Michelle, you’re awesome. Good job!" another nurse chimed in.
Perhaps the most amazing thing about the surgery, is Carpinelli will get to go home the next day.






