—Discover how opioid addiction affects the brain and how evidence based treatments are saving lives.—
We are in the midst of the deadliest drug epidemic in U.S. history.
In 2016, 64,000 Americans died from drug overdoses, driven by a dramatic rise in the abuse of opioids like OxyContin, heroin, and fentanyl.
Drugs are now the leading cause of death for people under the age of 50, and a key reason that life expectancy in the U.S. is falling after decades of gains.
It’s a slow-motion disaster that is destroying families and entire communities, with no end in sight. But what causes addiction, and why is it so challenging to treat?
NOVA takes an unflinching look at the science of addiction and how it works — traveling across the country to hear firsthand from individuals and families struggling with addiction and meet with researchers on the frontlines of the opioid crisis.
While addiction has long been viewed as a moral failing, leading scientists will help viewers understand why addiction is a disorder that occurs as drugs profoundly alter the brain.
As researchers gather scientific and clinical evidence, “Addiction” will explore how we might best address our drug problem, from advances in neuroscience, to the development of evidence-based treatments, to the rethinking of laws and public policies.
”Nearly every family in America has been affected by addiction — the biggest public health crisis facing us today; yet it remains poorly understood, largely stigmatized, and finding treatment can be a daunting process,” said Paula S. Apsell, senior executive producer, NOVA. “NOVA helps cut through the confusion by presenting the latest science on what we now know is a treatable brain disorder, and not a hopeless diagnosis.”
NOVA brings viewers on both a scientific investigation and an emotional personal journey — looking at the epidemic through the eyes of those living through it:
- In West Virginia, we meet Jasen and Mark Edwards, brothers from a rural coal mining community whose entire family has been devastated by the opioid crisis.
- NOVA also travels to California to meet “opioid refugee” Casey Greer, a young woman with a genetic vulnerability who inadvertently became addicted to prescription painkillers as a teenager following surgery to remove a benign tumor.
- In Vancouver, we’re introduced to Daniel, who turned to drugs to cope with the stress of prison.
- NOVA also spends time with a young mother striving to stay in recovery and reconnect with her young children in the foster care system, and takes viewers inside a neo-natal ward to see one of the most heartbreaking results of the epidemic.
- Every 22 minutes, a baby is born dependent on drugs. Dr. Stefan Maxwell, of Charleston Area Medical Center, cares for newborns with Neonatal Abstinence Syndrome and shares what the babies endure while going through the long and costly withdrawal process. Some families are coping with a loved one’s fatal descent into the spiral of addiction.
- In Virginia, NOVA meets with Former Vice Chairman of the Joint Chiefs of Staff, Admiral James “Sandy” Winnefeld (USN, Ret.), and his wife, Mary, who recently lost their 19-year-old son Jonathan to an accidental overdose of heroin and fentanyl — just after he had completed 15 months of costly and extensive in-patient rehabilitation and had appeared to be on solid ground. The couple has co-founded S.A.F.E. Project U.S., a nonprofit organization devoted to ending our country’s opioid epidemic.

Many think addiction is a choice and that stopping is simply a matter of willpower, but it’s much more complicated.
“Addiction” shows what it is and what it’s not through a series of experiments and the latest in brain imaging research.
Our brains are exquisitely tuned to seek rewards, explains Robert Malenka of Stanford University, so individuals struggling with addiction are battling millions of years of evolution.

Scientists discovered we have a “reward pathway,” which regulates emotions, movement, motivation, and memory, primarily controlled by a chemical messenger called dopamine. Dopamine is released when we eat, fall in love, or encounter anything exciting.
Addictive drugs can cause an unnatural rise in dopamine levels, generating one of the most powerful experiences our brains can have.

RELATED: Taking the Pain Out of Addiction By Leah Shaffer
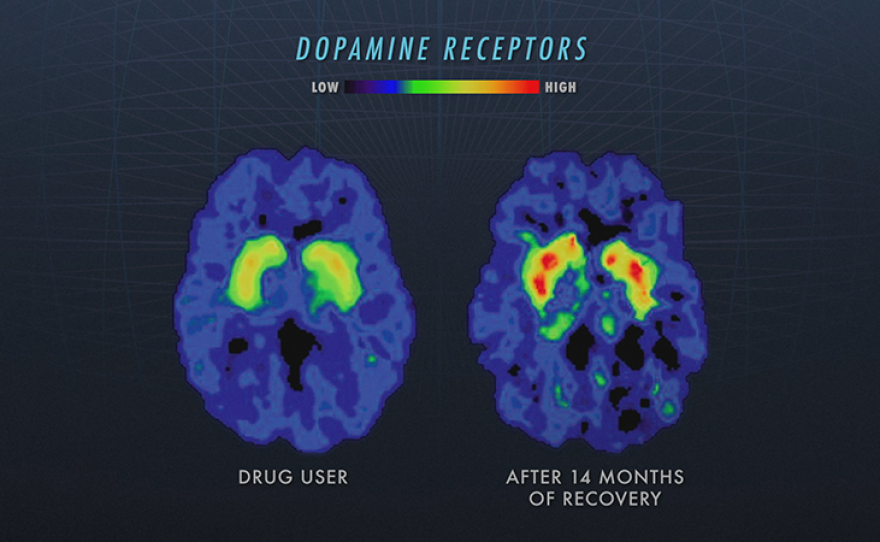
Dr. Nora Volkow, director of the National Institute of Drug Abuse, is investigating individuals addicted to different classes of drugs, and her brain imaging studies have found that one common change in brains exposed to drugs is a reduction in the levels of dopamine D2 receptors.
Fewer receptors means the brain is less responsive to dopamine. Dopamine is essential for motivation, and there is no way to magically produce dopamine in our brains in order to replace depleted levels.

For doctors like Dr. Corey Waller, of the National Center for Complex Health, the problem is that addiction is not handled like other diseases. He is a proponent of building a stabilized, evidence-based treatment system for addiction to intervene on the front end, rather than trying to fix everything that’s broken on the back end.
RELATED: Tracking Opioids Beneath the Streets by Kelsey Tsipis
He maintains that this will bring down the number of overdose fatalities and could also serve to bring down the high cost of medicine associated with drug, alcohol, nicotine addiction, and eating disorders — all of which account for a large portion of annual healthcare costs.
Currently, abstinence-based methods modeled on the Alcoholics Anonymous 12-step recovery program are prevalent in about 80 percent of American treatment centers. These can be effective tools for breaking isolation, providing peer support, and tackling addictions like alcoholism.
However, this approach has been shown to be unsuccessful in treating people with an opioid use disorder.
Growing evidence suggests that a more effective strategy for combating opioid addiction is medically assisted treatment, which serves to normalize brain functions altered by opioids, including dopamine levels.
Drugs like Methadone and Suboxone (a less potent medication that only partially activates the body’s opioid receptors) block the effects of heroin and pain pills, and decrease cravings.
Dr. Carrie Wilken, of Foundation for Change, says that programs that do not use these medications have an 80-to-90 percent failure rate in treating opioid addiction.
Studies also show that medications cut the risk of overdose death by half.
Tragically, evidence-based treatments are not widely available in the United States and patients and their families have to navigate a very broken system of care.
In Boston, Dr. Laura Kehoe, of Massachusetts General Hospital, runs one of the few programs in the U.S. that immediately offers overdose patients medications to control cravings. Kehoe says this strategy works: “We're seeing people come that day and engage in care, and the vast majority of them, 75 to 80 percent, are returning.”
Dr. James Berry, of WV University School of Medicine, also believes it’s time to take a new approach toward the treatment of opioid addiction. He initially prescribed Suboxone for short periods, but noticed that patients soon relapsed when they stopped. By keeping them on the medication for longer periods, he has seen patients stabilize, start to work again, and rebuild their lives.
RELATED: Finding Alternatives to Opioids by Caleb Hellerman
Harm reduction clinics are also helping to prevent the spread of infectious diseases and improve access to essential resources for those suffering from opioid addiction.
NOVA travels with Dr. Rahul Gupta, Commissioner & State Health Officer of the West Virginia Department of Health & Human Resources, to rural coal counties hit hard by the crisis.

Poverty and addiction in this region have brought a cascade of public health challenges. Gupta is trying to reverse the state’s soaring number of overdose deaths and hepatitis infections — among the nation’s highest — and prevent new outbreaks of HIV.
Traveling with a mobile clinic, Gupta and volunteer medical professionals with the non-profit Health Right, offer clean needles, Hepatitis C testing, drug counseling, and free naloxone, a drug which can stop an overdose.
According to Gupta’s analysis, every dollar spent on harm reduction saves up to seven dollars in medical costs and steers people towards treatment.
But Dr. Gupta also sees the big picture benefits: “The costs are unsustainable. We are losing over half a trillion dollars each year in our economy. We've got to be smart about addressing addiction and find ways to prevent it from happening in the first place.”
Vancouver, Canada is taking an even more radical approach. In 2003, it sanctioned the first legal, supervised injection program, where people can take illegal drugs in a safe environment monitored by healthcare professionals.
Called Insite, the program also provides clean needles, and its staff can reverse an overdose if one occurs. Insite also helps people test their drugs for fentanyl, as well as access services like treatment.
Highly controversial and still illegal in the United States, studies show that since Insite has opened, overdose deaths have plummeted 35 percent, and the number of HIV cases has declined dramatically in Vancouver.

Harm Reduction Manager Darwin Fisher says: “The most important things about supervised injection sites is that it implicitly says that these lives are worth saving, these people are valuable to us. People recover from addiction. Nobody is un-reclaimable. The only thing you can’t recover from is death.”
For Stanford psychiatrist Anna Lembke, the way is clear. To tackle an issue of this magnitude, there is not one path to the top of the mountain. We now have several treatment options and must make all of them available in order for people to thrive. “The solution is for us to embrace addiction as a disease and bring it within the house of medicine, so anybody struggling with addiction can walk into an emergency room or pediatrician’s office, and say, ‘I’m having a problem with drugs or alcohol, will you help me?’ And the answer is an enthusiastic, ‘YES!’”
More About Addiction, Prevention, And Recovery:
NOVA will present an interactive, online piece of multimedia content that allows users to engage with data and journalism related to the content presented in the film. The interactive will be published on NOVA’s website on Oct. 17, 2018, and will weave together video, audio, visuals, and data to tell a compelling and actionable story about addiction, prevention, and recovery.
NOVA is excited to partner with High Intensity Drug Trafficking Area (HIDTA) to showcase how data is being used to save lives — whether by partnering with law enforcement to know where to find dealers or to head off an overdose outbreak before it kills more people.
Watch On Your Schedule:
Episodes are available for viewing on demand for a limited time after each broadcast. Extend your viewing window with KPBS Passport, video streaming for members ($60 yearly) using your computer, smartphone, tablet, Roku, AppleTV, Amazon Fire or Chromecast. Learn how to activate your benefit now.
Join The Conversation:
NOVA is on Facebook, and you can follow @novapbs on Twitter. #NOVAnext
Credits:
A NOVA production for WGBH Boston. Written, directed, and produced by Sarah Holt. Deputy Executive Producer for NOVA is Julia Cort. Senior Executive Producer for NOVA is Paula S. Apsell.





